top of page
Policy Project
The Step Two Policy Project is a policy think tank that focuses on issues involving health, behavioral health, and human services in New York. Our goal is to make complicated subjects more understandable to general readers, while providing detailed insights for people who work in the health policy field.
The Affordable Care Act at the Brink – Part II: Evaluating the HSA Construct
By Paul Francis with Adrienne Anderson
December 29, 2025
To read the Issue Brief, click here.
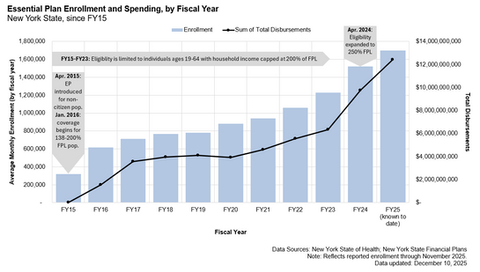
New: Enrollment and State Spending Data Visualizations
bottom of page